Elbow Stability and Movement Coordination Impairments
Ulnar collateral ligament (UCL) pathology often occurs in individuals who perform repeated/forceful overhead movements. If your patient is an overhead athlete complaining of medial elbow pain, check the UCL!
If you do not know the common clinical findings no problem! Click here
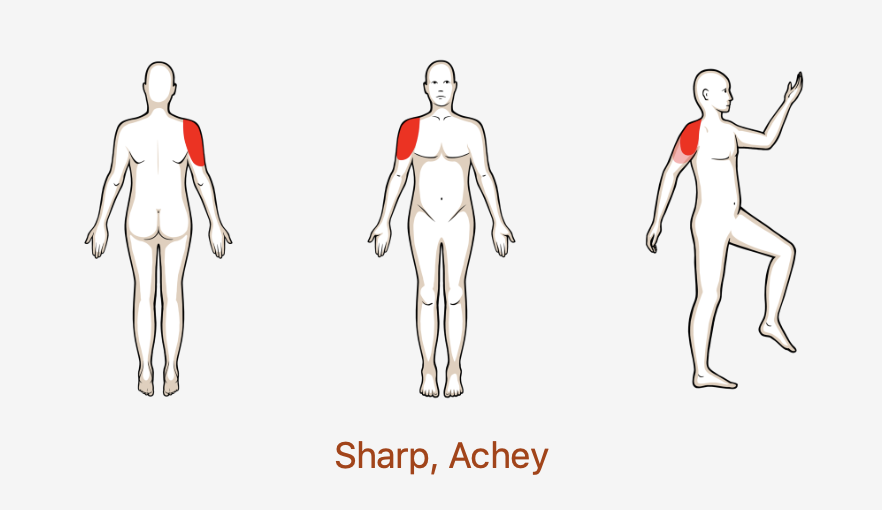
Anatomy
Image via Complete Anatomy 2018 by 3D4 Medical
Key Finding
Palpation of the UCL can help to assess if the UCL is indeed a pathological source tissue. If radicular symptoms are present upon palpation, especially in in the 4th and 5th digits, there could be ulnar nerve involvement as well! (Click image to watch 1-2 minute video)
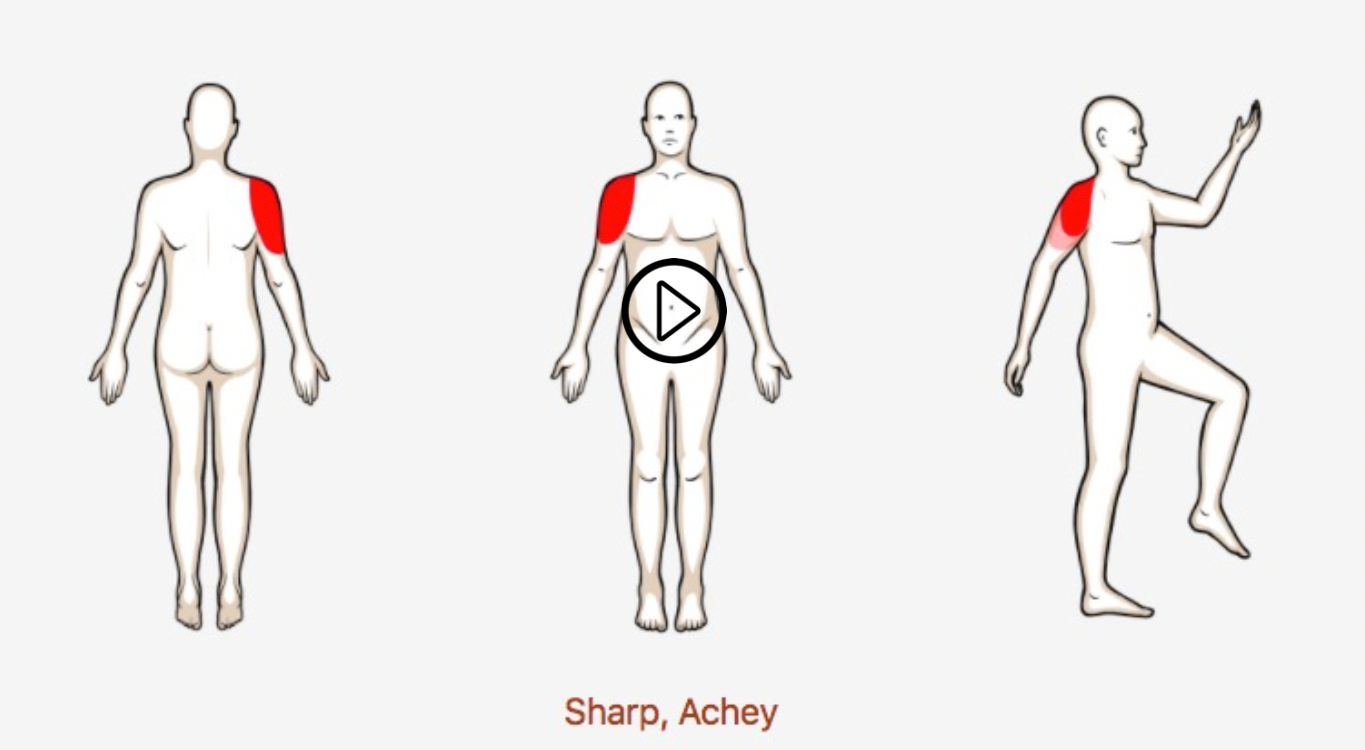
Movement Fault
In overhead athletes, decreased shoulder external rotation range of motion can result in increased valgus stress directed at the UCL! (Click image to watch 1-2 minute video)
Clinical Pearl: In overhead athletes it is important to assess the entire kinetic chain in order to determine if faulty force transmission is present. For example, research shows that decreased hip internal rotation range of motion can also result in excessive force transmission through the shoulder and the elbow!
Special Test
The moving valgus stress test is excellent for ruling out UCL pathology with a sensitivity of 100! Take a look and see how its done! (Click image to watch 1-2 minute video)
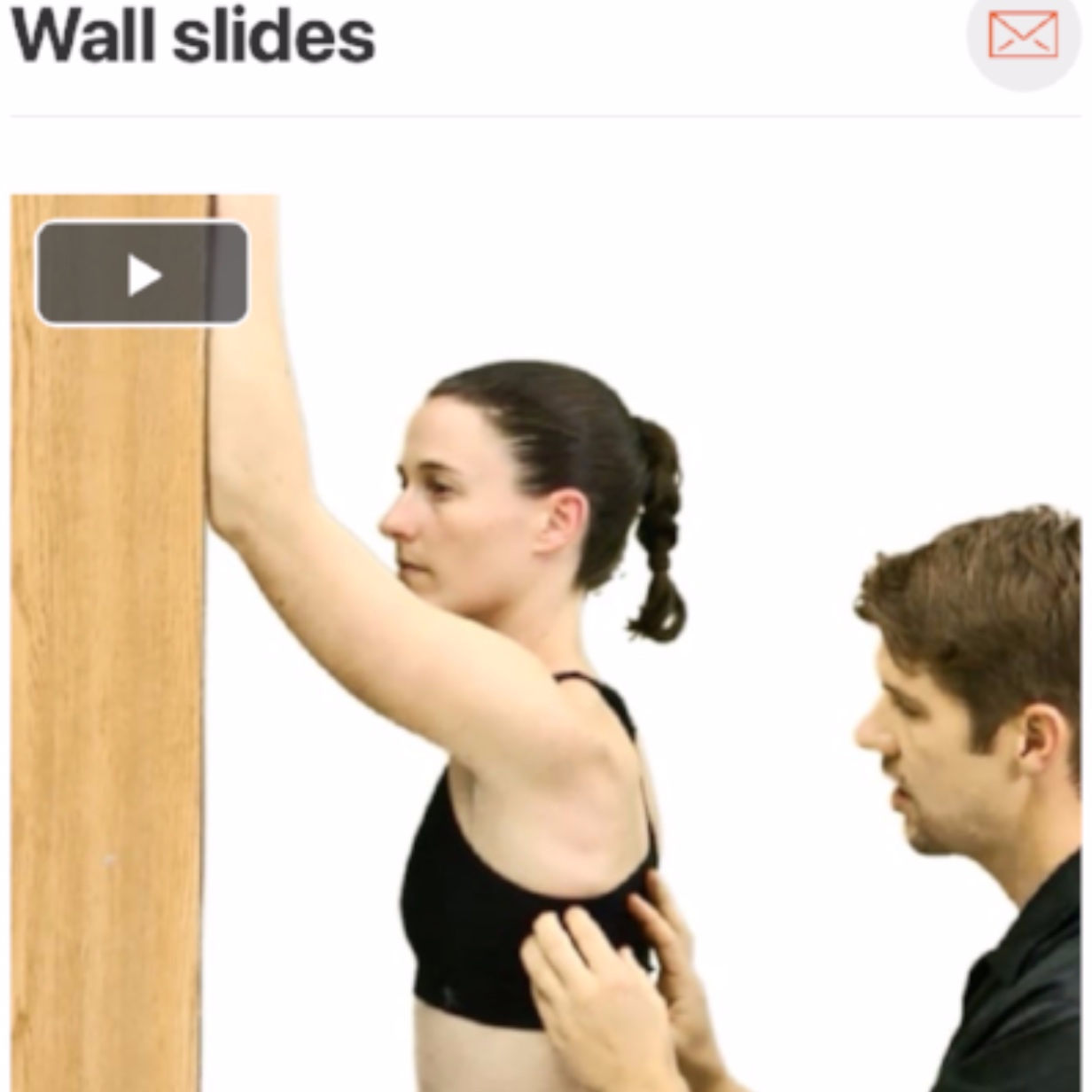
Treatment/Therapeutic Exercise
Research suggests that in overhead athletes, the posterior aspect of the glenohumeral joint capsule can often contracture due to high rates of repetitive movement. This change in tissue can result in limited shoulder range of motion and subpar shoulder arthorokinematics potentially leading to increased strain on structures like the UCL! The patient can also be taught how to perform this exercise at home! (Click image to watch 1-2 minute video)
*Acutely, addressing pain and inflammation around the UCL via techniques such as soft tissue mobilization and activity reduction may prove to be beneficial.